How Big Pharma Abuses the Healthcare System
On December 10th, 2021, the U.S. House of Representatives Committee on Oversight and Reform released a 192-page report on the pharmaceutical industry’s pricing and business practices. Over the nearly three year investigation, they reviewed more than 1.5 million pages of internal company documents. In short, the report concludes what people with diabetes have known their whole lives: that Big Pharma abuses the healthcare system to increase profits at the expense of patients.
“The result of the House Oversight Committee investigation is clear: American families are suffering from outrageous drug prices, while Big Pharma rakes in record profits.”
— House Speaker Nancy Pelosi (D-CA)
These are the same corporations that many diabetes-focused nonprofits like the Juvenile Diabetes Research Foundation (JDRF), American Diabetes Association(ADA), and Beyond Type 1 have cozied up to, raking in millions of dollars in exchange for silence on (and support of) these abuses. Now, the record is clear: Big Pharma is not on the side of people with diabetes. So why are so many nonprofits willingly in their pockets?
The tweet above from the House Oversight Committee states: We’re not done - One of the documents uncovered by our investigation shows that one Novo Nordisk employee wrote “all I want for Christmas” is for insulin manufacturers to increase their prices in lockstep. - This is shameful.
Highlights
Drug companies (Eli Lilly, Novo Nordisk, and Sanofi were specifically called out) use a variety of strategies to suppress competition:
Abusing the patent system to stop competition (12 drugs examined had over 600 patents, potentially extending the monopolies to a combined 600 years)
Shifting patients to newer drugs before the generic form of older products is released
Adding conditions to pharmacy benefit manager (PBM) rebates that exclude competitor products on formularies
Aggressively marketing their drugs to patients and doctors when there are generic options
Using “shadow pricing” to follow their competitors’ price increases
The graph above shows the identical increase in insulin prices across the two most popular brand name insulins, Novolog and Humalog. Eli Lilly and Novo Nordisk exponentially increased the price of each insulin at the same time as the other. Novolog was introduced in 2001 at around $45. By 2018, both brands were charging close to $300 per vial.
Medicare
The Committee found that Eli Lilly, Novo Nordisk, and Sanofi, whom control nearly 100% of the insulin market in the U.S., provided private Medicare Part D plans with significantly smaller rebates than those by other federal health care programs, costing patients US$16.7 billion from 2011-2017.
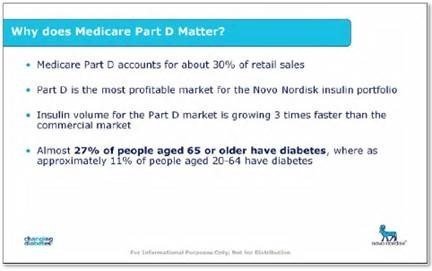
An internal document from Novo Nordisk, below, clearly shows their strategy for Medicare plans.
The image above, an internal document from Novo Nordisk, states: Why does Medicare Part D Matter? 1. Medicare Part D accounts for about 30% of retail sales, 2. Part D is the most profitable market for the Novo Nordisk insulin portfolio, 3. Insulin volume for the Part D market is growing 3 times faster than the commercial market, and 4. Almost 27% of people aged 65 or older have diabetes, whereas approximately 11% of people aged 20—64 have diabetes.
Price Increases
The 12 drugs examined are now priced, on average, 500% higher than when they were brought to market. Humalog, for example, has increased 1171% from January 1997 to December 2017.
The image above shows an internal document from Novo Nordisk which states: Top two questions we always hear from you. We’re always looking to improve our approach and welcome your feedback.
Question 1: Why do we keep raising list prices? Answer: Management expects 10%+ YoY growth; Payer negotiations focused on net price; Non-contracted volume optimization
Question 2: Why can’t we go after more accounts? Answer: Sanofi and Lilly able and willing to fight back; Volume upside at much lower margins; Price war = steep price erosion
Drug companies specifically target the U.S. market for increased prices, while maintaining or lowering prices in other countries. Eli Lilly, for example, makes twice the revenue from all of its diabetes drugs in the U.S. as the rest of the world combined ($2.1 billion vs $1.1 billion in Q3 2021).
The data table above shows 2021 revenue for Eli Lilly’s diabetes drugs: Baqsimi, Basaglar, Glucagon, Humalog, Humulin, Jardiance, Trajenta, and Trulicity. Across each quarter, they made twice the amount in the U.S. ($2.1 billion Quarter 3) as the rest of the world combined ($1.1 billion Quarter 3).
Eli Lilly, for example, makes twice the revenue from all of its diabetes drugs in the U.S. as the rest of the world combined.
Research & Development
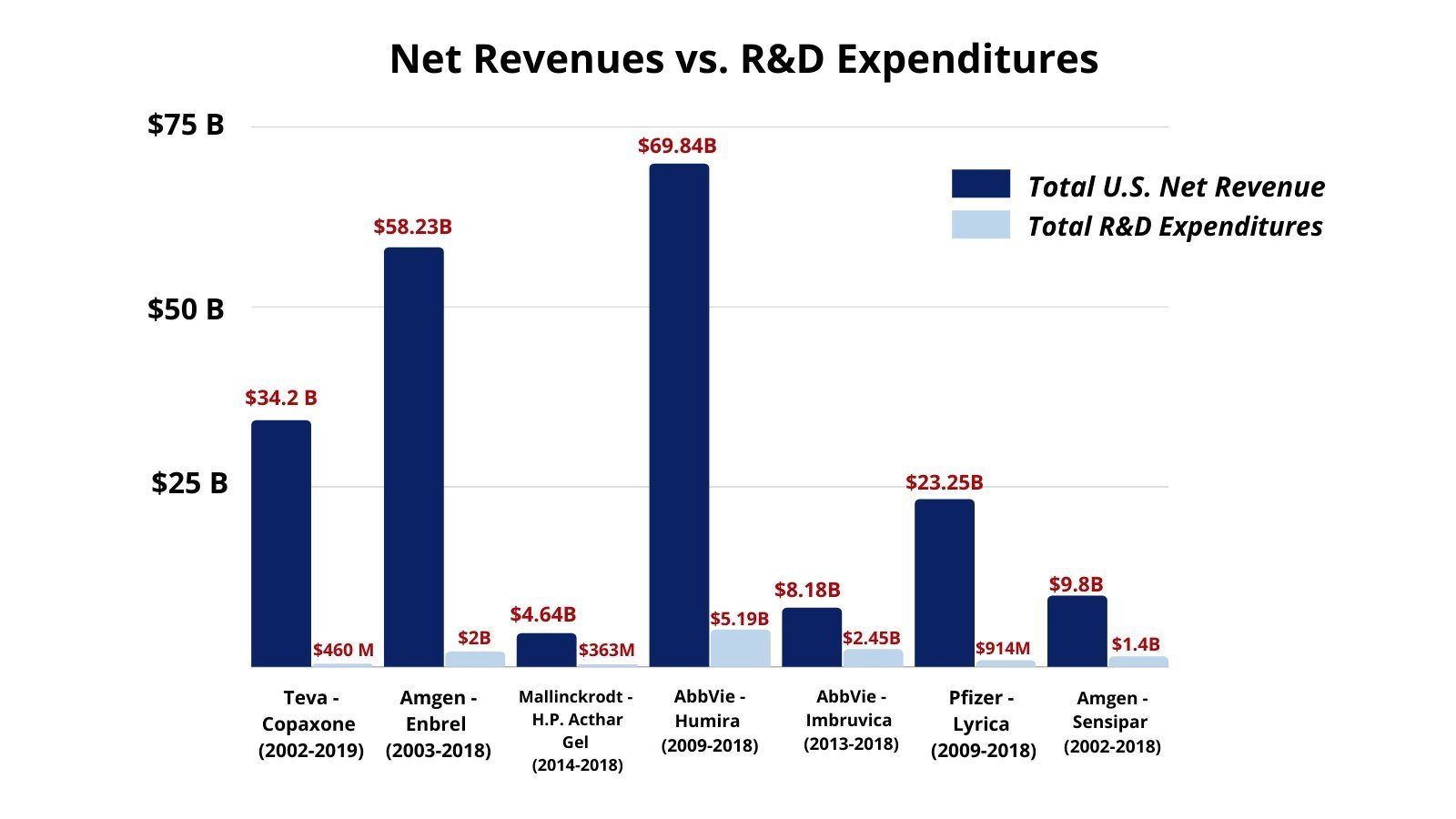
Drugmakers argue that they need increasingly high prices to pay for their research and development (R&D), but the investigation found that revenue gains far exceeded the R&D costs. From 2016-2020, the 14 leading drug companies spent US$577 billion on stock buybacks and dividends—US$56 billion more than they spent on R&D. Additionally, a signification portion of those R&D costs were spent on finding ways to extend their market monopolies and suppress competition, not new drugs.
The graph above shows Net Revenues vs. R&D Expenditures for several big pharmaceutical companies: Teva, Amgen, Mallinckrodt, AbbVie, and Pfizer. On the lower end, Amgen spent $1.4 billion on R&D for Sensipar compared to $9.8 billion in revenue. On the higher end, AbbVie spent $5.1 billion on R&D for Humira compared to $69.8 billion in revenue.
Drugmakers argue that they need increasingly high prices to pay for their research & development (R&D)… but their revenue gains far exceeded R&D costs… and a significant portion of those R&D costs were spent on finding ways to extend market monopolies… not new drugs.
Executive Compensation
Every company the Committee looked into tied executive compensation (bonuses) to hitting revenue targets. That means, employees are financially incentivized to increase the price of drugs so that they can personally make more money (at the expense of patients).
The data table above shows the average Executive Committee Compensation for 2016-2020. The total for the top insulin manufacturers were as follows: Eli Lilly at $234,015,759; Novo Nordisk at $123,812,234; and Sanofi at $60,467,284.
Employees are financially incentivized to increase the price of drugs so that they can personally make more money.
Patient Assistance Programs
The Committee found that patient assistance programs are a public relations tool to boost sales. Drug companies make much more money on these programs than it costs them, sometimes at a 4.5x return. These programs do not provide sustainable support for patients and don’t address the fact that people are relying on these programs because of the drug companies’ own abuses.
Note: One of the biggest arguments against Beyond Type 1’s GetInsulin.org (besides the fact that it does not work for many people) is that it’s a public relations campaign for drugmakers’ “charitable” patient assistance programs that only need to exist because the drug makers price 1-in-4 Americans out of purchasing insulin—and then the drugmakers make money from these programs.
“Our investigation shows that @PhrMA uses patient assistance programs as smokescreens to keep drug prices high.”
— Committee on Oversight and Reform
What Can We Do?
The only way to limit Big Pharma’s monopoly over our lives is to limit their power through legislation. You can visit, write to, or call your Senators and Representatives and demand that they protect YOU instead of drugmaker profits:
Senators are pushing to change the $35 co-pay cap for insulin in the Build Back Better Act to a $35 price cap (which would cover everyone, even if they don’t have insurance).
The Affordable Prescriptions for Patients Through Promoting Competition Act addresses anticompetitive practices like targeting doctors to prescribe name-brand drugs instead of generics.
The Preserve Access to Affordable Generics and Biosimilars Act stops drugmakers from paying other companies to delay their generic and biosimilar drugs from entering the market.
Forcing companies to be transparent about their R&D costs to see if cost increases are actually justified (or just an excuse to make more money).
Are the above facts upsetting to you? Contact Your Senators & Representatives
Contact your representatives and ask them to fight for affordable insulin. We have a pre-filled letter to make this process easier for you.